
Jiemin Ma, PHD, MHS, Strategic Director,
Surveillance and Health Services Research, American Cancer Society
(443) 804-7314; [email protected]
On behalf of the ACS (this year’s lead agency), I’m pleased to announce that the latest Annual Report to the Nation on the status of cancer (ARN) was published on March 31, 2017. This is the 19th “edition” of ARN, which represents an annual collaborative effort by the ACS, CDC, NAACCR, and NCI. This would not have happened without the great inputs from each of the collaborators and the contributions of the state and regional cancer registry staff who collected the data.
 During 1999-2013, the overall cancer incidence rates continued to decrease among men and remained stable among women. The overall cancer death rates continued to decline during 2000-2014 among men, women, and children. The decreases in death rates are the continuation of trends over the past 20 years. Factors that have contributed to these decreasing trends include reduced tobacco use, improved early detection (e.g., colorectal, breast, and cervical cancer), and improved treatments for many cancers. In particular, due to public health policies against tobacco and increased awareness of the health hazards of smoking, adult smoking prevalence has decreased by over 50% over the past five decades. However, tobacco use still accounts for nearly one-third of cancer deaths in the U.S. and about 40 million of Americans still smoke. These facts underscore the need for expansion of tobacco control programs and the development of new strategies to accelerate the reduction in tobacco use.
During 1999-2013, the overall cancer incidence rates continued to decrease among men and remained stable among women. The overall cancer death rates continued to decline during 2000-2014 among men, women, and children. The decreases in death rates are the continuation of trends over the past 20 years. Factors that have contributed to these decreasing trends include reduced tobacco use, improved early detection (e.g., colorectal, breast, and cervical cancer), and improved treatments for many cancers. In particular, due to public health policies against tobacco and increased awareness of the health hazards of smoking, adult smoking prevalence has decreased by over 50% over the past five decades. However, tobacco use still accounts for nearly one-third of cancer deaths in the U.S. and about 40 million of Americans still smoke. These facts underscore the need for expansion of tobacco control programs and the development of new strategies to accelerate the reduction in tobacco use.
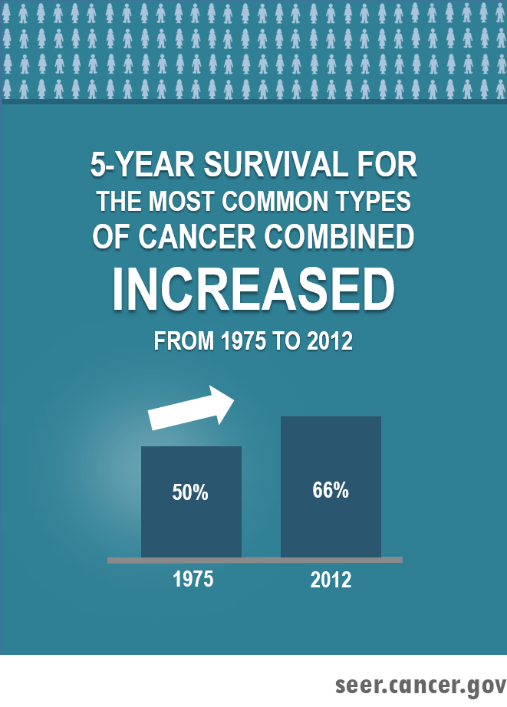 This year’s ARN features cancer survival. Reflected by a 16% absolute increase in 5-year relative survival from 1975-1977 to 2006-2012 for all cancers combined, the overall cancer survival has been improving over the past four decades. By cancer site, the greatest absolute increases in survival rate were found for cancers of the prostate, kidney, NHL, myeloma, and leukemia. Both advances in treatment and declines in surgical mortality may have contributed to the improvements in survival. However, no improvements in survival have been found for cancers of the cervix and uterus. Five-year relative survival remained low for some cancer sites such as pancreas (8.5%), liver (18.1%), lung (18.7%), and esophagus (20.5%).
This year’s ARN features cancer survival. Reflected by a 16% absolute increase in 5-year relative survival from 1975-1977 to 2006-2012 for all cancers combined, the overall cancer survival has been improving over the past four decades. By cancer site, the greatest absolute increases in survival rate were found for cancers of the prostate, kidney, NHL, myeloma, and leukemia. Both advances in treatment and declines in surgical mortality may have contributed to the improvements in survival. However, no improvements in survival have been found for cancers of the cervix and uterus. Five-year relative survival remained low for some cancer sites such as pancreas (8.5%), liver (18.1%), lung (18.7%), and esophagus (20.5%).
Racial disparities in survival have persisted over time for many common cancers, although improved survival was found among both blacks and whites. In addition, cancer survival varied considerably across ethnic groups and states. For example, after adjusting for sex and age, the risk of death for all cancers combined was 33% (HR=1.33) higher in non-Hispanic blacks and 51% (HR=1.51) higher in non-Hispanic American Indians/Alaska Natives compared with non-Hispanic whites. These findings remind us that more efforts should be made to discover new strategies for prevention, early detection, and treatment and to apply proven interventions broadly and equitably.
Press Release | FAQ | Contact Us
Abstract
Background
The American Cancer Society (ACS), the Centers for Disease Control and Prevention (CDC), the National Cancer Institute (NCI), and the North American Association of Central Cancer Registries (NAACCR) collaborate to provide annual updates on cancer occurrence and trends in the United States. This Annual Report highlights survival rates.
Methods
Data were from the CDC- and NCI-funded population-based cancer registry programs and compiled by NAACCR. Trends in age-standardized incidence and death rates for all cancers combined and for the leading cancer types by sex were estimated by joinpoint analysis and expressed as annual percent change. We used relative survival ratios and adjusted relative risk of death after a diagnosis of cancer (hazard ratios [HRs]) using Cox regression model to examine changes or differences in survival over time and by sociodemographic factors.
Results
Overall cancer death rates from 2010 to 2014 decreased by 1.8% (95% confidence interval [CI] = –1.8 to –1.8) per year in men, by 1.4% (95% CI = –1.4 to –1.3) per year in women, and by 1.6% (95% CI = –2.0 to –1.3) per year in children. Death rates decreased for 11 of the 16 most common cancer types in men and for 13 of the 18 most common cancer types in women, including lung, colorectal, female breast, and prostate, whereas death rates increased for liver (men and women), pancreas (men), brain (men), and uterine cancers. In contrast, overall incidence rates from 2009 to 2013 decreased by 2.3% (95% CI = –3.1 to –1.4) per year in men but stabilized in women. For several but not all cancer types, survival statistically significantly improved over time for both early and late-stage diseases. Between 1975 and 1977, and 2006 and 2012, for example, five-year relative survival for distant-stage disease statistically significantly increased from 18.7% (95% CI = 16.9% to 20.6%) to 33.6% (95% CI = 32.2% to 35.0%) for female breast cancer but not for liver cancer (from 1.1%, 95% CI = 0.3% to 2.9%, to 2.3%, 95% CI = 1.6% to 3.2%). Survival varied by race/ethnicity and state. For example, the adjusted relative risk of death for all cancers combined was 33% (HR = 1.33, 95% CI = 1.32 to 1.34) higher in non-Hispanic blacks and 51% (HR = 1.51, 95% CI = 1.46 to 1.56) higher in non-Hispanic American Indian/Alaska Native compared with non-Hispanic whites.
Conclusion
Cancer death rates continue to decrease in the United States. However, progress in reducing death rates and improving survival is limited for several cancer types, underscoring the need for intensified efforts to discover new strategies for prevention, early detection, and treatment and to apply proven preventive measures broadly and equitably.
The opinions expressed in this article are those of the authors and may not represent the official positions of NAACCR.
